What is ICD 10? – Overview
Are you a healthcare professional looking for information on ICD 10?
In October 2015, clinics and other healthcare systems were mandated to use a new E&M coding format, ICD-10, for years.
Although most medical professionals dreaded the change, it was necessary and had been long unresolved.
The formal international release of ICD-11 is still scheduled for 2022, implying that the eventual change to yet another ICD coding system in the United States is only a few years away.
With that in mind, it’s worth looking at the current condition of ICD codes, the function of ICD-10, and where the system could still be improved.
Until 2015, the United States healthcare system had relied on ICD-9 since 1979. However, Healthcare is constantly evolving, and today’s healthcare needs differ from those of 40 years ago.
Some ICD-9 codes were outdated and did not even reflect modern medical procedures.
It provided minimal information about a patient’s medical condition, and the ICD-9 format restricted the number of additional codes that could be added, as many ICD-9 categories were already filled.
As a result, a new coding technique has been implemented. Now, are you wondering, “What is ICD 10?” If so, then read below.
What is ICD 10?
ICD-10 is the World Health Organization’s tenth update to the International Classification of Diseases (ICD) (WHO).
The International Classification of Diseases (ICD) provides the foundation for containing health trends and the global standard for reporting illnesses and disorders.
ICD codes are used by providers and infirmaries worldwide to describe symptoms, diseases, and injuries, and insurance companies utilize that data to process claims.
ICD-10 Codes
| ICD-10 Codes |
|---|
| ICD 10 Code for Depression |
| Hyperlipidemia ICD-10 |
| ICD-10 Anemia |
| ICD-10 GERD |
| ICD-10 UTI Coding System |
| Breast Cancer ICD-10 |
| ICD-10 Dysphagia |
| ICD-10 CAD Coding |
The Importance of ICD-10
ICD is an abbreviation for the International Classification of Diseases. ICD-9-CM was introduced more than 30 years ago, and today’s healthcare data requirements are vastly different from those of the 1970s.
As a result, ICD-9 cannot appropriately define diagnoses and inpatient treatments for the provided care.
Electronic health record providers and hospital systems who have effectively integrated Isabel into their workflow using ICD-9 will reap numerous benefits from switching to ICD-10, promoting Healthcare in various ways.
Quality Assessment
ICD-10 provides more depth and a higher capacity to handle new technology and treatments, allowing for the more significant growth of codes for medical complications and medical safety risks.
Furthermore, better documented, collected, and assessed data informs better clinical decisions between Isabel and the integrated system.
Complete, accurate, and up-to-date procedure codes will improve new medical technology’s data, efficacy, and costs while ensuring fair reimbursement for its use.
In addition, using Isabel’s ICD-10 coding with your system will ensure that any diagnoses established using Isabel in your clinical workup are effectively reimbursed.
Public Health Changes
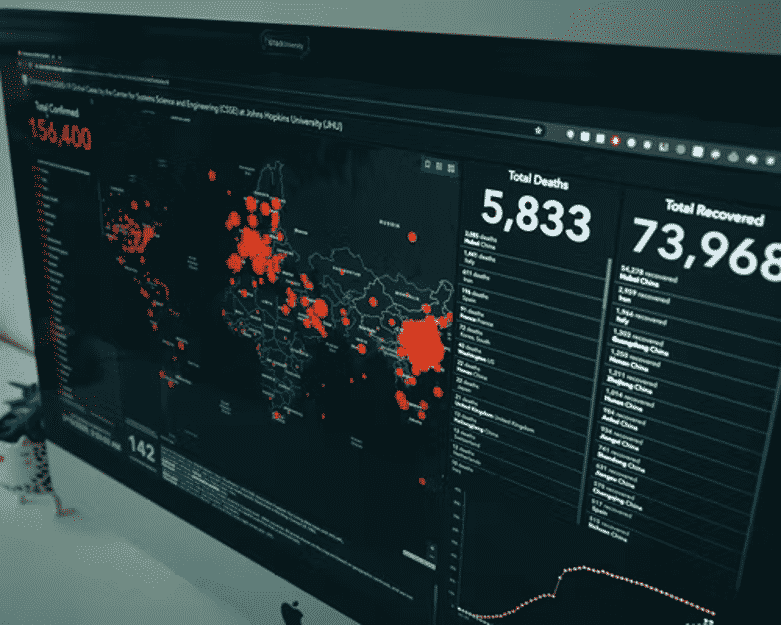
With the introduction of ICD-10 into the US market, the US will share morbidity data internationally and track and respond to global hazards in real-time.
It can also connect public health trends to global pandemics, influencing public health policy.
ICD-10 is more effective than ICD-9 at capturing public health diseases.
It is more specific and fully catches more nationally reportable public health diseases and those connected to the top ten causes of mortality and bioterrorism.
Research Impact
The ICD-10 code is more structured and easier to navigate than the ICD-9 code, and it is believed that this would lead to better coding decisions.
It enables precise classification of the “type of injuries,” linking them with cause, treatment, and outcome.
Code analysis is a vital research component when there is no direct access to patient medical information.
Greater visibility provided by accurate ICD-10 classification allows for discovering previously hidden links or discovering phenomena such as early forming epidemics.
This will address the pandemic head-on, lowering the expenses of late diagnosis and avoiding consequences connected with the epidemic.
In addition, ICD-10 coding will help formulate procedures and clinical pathways for medical diseases.
Essential Health IT Advancement
Upgrading to ICD-10-CM will allow the full potential of Health IT to be fulfilled. ICD-10 data is more accessible to obtain in electronic format than ICD-9 data.
Since the code set is more robust and current, it provides fine-mapping to SNOMED CT, which captures the clinical detail of a care episode. (In addition, Isabel provides SNOMED CT coding.)
These mapping systems improve uniformity, efficiency, and accuracy by facilitating Computer-Assisted Coding (CAC).
Shifting from ICD-9 to ICD-10 offers a more robust and detailed approach. Upgrade your Isabel integration to ICD-10 to stay ahead of the curve in health IT.
Reimbursement Changes
Because of the increase in ICD-10-CM codes provides a better framework for creating payment systems.
Accurate payments for new technology procedures should help ICD-10 because these operations could be uniquely identified.
Professionals can discover risk adjustments in ICD-10 categories to capture patient behavior such as smoking, alcohol consumption, poor nutrition, and exercise routines.
As more ICD-10 codes become accessible, it becomes easier to verify reported codes with clinical documentation, check for consistency between diagnosis and procedures prescribed, and look for nonsensical diagnoses combinations.
This will help decrease fraud and eliminate the coding gray areas in ICD-9.
Significant Changes in ICD-10-CM:
- Anatomy’s Importance: Injuries are classified according to their anatomical location rather than their type.
- Consolidation of E and V Codes: The ICD-9-CM V codes (Factors Influencing Health Status and Contact with Health Services) and E codes (External Causes of Injury and Poisoning) are incorporated into the main classification separated into additional categories as they were in ICD-9-CM.
- Unique descriptions: In some cases, new code characterizations are offered to match modern medical practice (e.g., the purpose of acute myocardial infarction is now four weeks rather than eight weeks).
- Classification restructuring and code reorganization have emerged in various ICD-10-CM chapters, classifying certain illnesses and disorders that differ from ICD-9-CM.
- Revaluation: Specific diseases have been reclassified to other chapters or sections to reflect current medical understanding.
Improved Care Quality
One of the essential benefits of ICD-10 is its ability to offer exact and thorough data to providers.
ICD-10 codes, for example, indicate laterality, stage of care, accurate diagnosis, and comprehensive anatomy, resulting in a more precise picture of the patient’s disease.
This enables the provider to allocate appropriate care and resources, resulting in improved outcomes.
In addition, proper documentation of a patient’s diagnosis leads to a more relevant healthcare understanding.
It is helpful for other providers who will access the patient’s health information in the future. It also means improved patient safety and fewer requests for paperwork to support diagnosis from payers.
Developing Health Approaches
ICD-10 was also developed to aid public health. It can assist healthcare organizations in collecting public health disease data, tracking global health concerns, responding to early pandemic tendencies, and developing improved healthcare policy.
Furthermore, it provides data to measure and track healthcare utilization and patient care quality and establish preventative care and disease management programs.
Fewer Reimbursement Refusals
The precision in ICD-10 codes helps eliminate billing errors and misunderstandings, resulting in fewer rejected claims.
It also minimizes the number of claims denied due to a “lack of medical necessity.” The faster you can get reimbursed, the more efficient the claims processing process is.
Improved Research Data
This specificity is also helpful for analysis. For example, ICD-10 codes can help reveal previously unknown linkages between health disorders, saving thousands of lives and billions of dollars in medical care costs.
In addition, in clinical research trials, ICD-10 codes lead to better data collection, adverse outcomes, and outcome evaluation reporting.
Acceptable Payments
Because ICD-10 gives greater detail about medical problems and services provided, it assists payers and legislators in improving our present reimbursement system and implementing pay-for-performance schemes.
Furthermore, because ICD-10 is more granular than prior editions, patients are appropriately invoiced for the therapy received, and physicians are fairly compensated for their services.
Fraud Control
Consequently, ICD-10 codes can help uncover potential fraud and inflated claims, lowering medical care expenses.
Furthermore, the system allows you to check for contradictions between strategy codes and diagnoses and irrational code combinations.
More sporadic shady areas in medical billing make it difficult for fraudulent people to conceal obscurities or flaws in code descriptions.
ICD-10 Additional Benefits
Substituting ICD-9-CM for ICD-10-CM and ICD-10-PCS, which handle procedure codes, will give higher-quality data for assessing healthcare service quality, safety, and efficacy.
Furthermore, this will provide more relevant data to:
- Improved Quality and Reduced medical mishaps (patient safety).
- Measuring outcomes and Health policy development.
- Measurement of clinical, monetary, and administrative implementation
- Operational and strategic planning, as well as the design of healthcare delivery systems
- Payment system design and claim processing
- Reporting on the use and impact of modern medical technologies.
- Improvements to existing reimbursement systems, such as severity-adjusted DRG systems.
- Pay-for-performance schemes and managed Care processes.
- Educating patients about the costs and results of various treatment options.
Updating to the most current code sets will also increase efficiencies and lower administrative costs due to replacing a malfunctioning classification system. As a result, this authorizes:
- Advanced use of automated methods to speed up the coding process.
- Costs associated with claim submission or adjudication are reduced.
- Rejecting unsuitable refund claims is becoming more common.
- Manual examination of health logs is no longer required to meet the information needs of payers, researchers, and other data mining purposes.
- Significant research organizations are no longer required to maintain separate classification systems (reimbursement and research).
- Reduced labor costs and increased productivity.
- Increased ability to deter and detect healthcare fraud and abuse.
By analyzing the dollar value of the benefits in the following classifications, it has become clear that the benefits considerably outnumber the execution costs:
- More precise compensation and fewer claims were rejected.
- Improved comprehension of new techniques
ICD 10 Transition Effects
The change will be challenging, and even the most well-prepared office may encounter issues immediately following the shift.
Prepare for a drop in productivity and accuracy and the need for further training and education.
See Also ICD 10 Coding Training for Physicians
In addition, expect claims processing delays and an increase in the number of denied claims, but remember, “no pain, no gain.”
ICD-10 Transition Guidelines
In general, the eight measures outlined below will aid in the successful deployment of ICD-10 this year:
1. A physician should lead the transition team, including the practice executive, coders, other office personnel, and medical assistants. In addition, those responsible for documenting the medical record must be involved and begin training as soon as possible.
2. There are several plans in this category, including one for education and training, one for assessing current documentation, one for completing a gap analysis, and one for implementation.
This year, keep an eye out for and participate in the AAOS educational program on ICD-10 transition and implementation. Then, execute your plans once you’ve formulated them.
3. A qualified specialist or team should select the top 25 to 40 diagnoses seen in the practice. Then, the team should code the identical instances to ICD-10-CM using current documentation and see what is lacking.
4. Send office personnel to a seminar or hire a consultant to provide specialized onsite training in orthopedics or other business specialty areas.
5. Change the template for your electronic health record system. Capture the information required for the best and most specific code to choose.
6. Identify all locations where ICD codes are used because they all need to be altered. Take advantage of the chance to improve processes.
7. Continue your training, as it is not a one-time event; it must be done regularly.
8. Be the physician champion in your practice who supports this move and can provide a detailed diagnostic or diagnosis for coding.
Who Benefits From ICD 10?
ICD 10 is an administrative load for the Medics; systems require coding in the new language. However, the physician’s role is to diagnose and treat patients.
Coding the patient will eventually benefit from correct diagnosis, effective treatment, and, ideally, lower costs by allocating the proper codes and streamlining the procedure with ICD-10.
Furthermore, ICD-10 will collect specific and factual data to assist physicians in their professional Maintenance of Certification reporting across the specialties of patients they have cared for.
Because technology has advanced, it is only natural that the coding methods used in the United States for Healthcare reflect this and, at long last, become up to current.
ICD-10 Frequently Asked Questions
What is ICD 10?
ICD-10 is international classification of diseases proposed by world health organization to report illness and disorders in alphanumerical codes.
What is alphabetical index in ICD-10?
Alphabetic index in ICD-10 book is for Anatomical sites or histology.
What is the main function of ICD-10?
ICD-10 is international classification of diseases proposed by world health organization to report illness and disorders in alphanumerical codes.
What is the purpose of ICD-10?
It enhances the quality of data for tracking health conditions and also provide help physicians and other healthcare professional to classify and code the diseases and medical conditions.
Who Benefits From ICD 10?
Physicians, healthcare professionals, patients and insurance benefits from ICD-10. Coding the patient will eventually benefit from correct diagnosis, effective treatment, and, ideally, lower costs by allocating the proper codes and streamlining the procedure with ICD-10.
Conclusion
Assume you’re searching for hands-on ICD-10 training and materials to assist you in navigating the shifting diagnosis coding landscape in your profession or career.
Then we hope that this article helps you. We ensure that you get the basics about what ICD 10 is and how it is important.
Furthermore, we also added who can attain the benefits from it and what the changes that it brought to the codecs. Hope this article helps you.
See Also
Integrative Medicine Traning for Physicians
4 Week Online Course for Medical Billing and Coding
Medical Billing and Coding Salary