Popular Names of Blood Thinners And How They Work – Introduction
Several medicines and drugs are prescribed to us for our smooth and healthy functioning. Even if these medicines are for your improvement, it is best to know how they function and understand their mechanism once we take them.
Blood thinners or anticoagulants work to disrupt the formation of clots in your bloodstream. They have a distinct mechanism of action, where they act on different pathways of the coagulation cascade to ensure that the blood flow remains smooth and without the formation of any clots or ‘thrombi’ that may otherwise pose a risk for the development of harmful diseases.
This article will review the names and overview of commonly used blood thinner medications. We will also briefly discuss the steps of the coagulation cascade to enhance our understanding of how they work.
Names of Blood Thinners Used in Common Practice
With the recent advancements in medical sciences, several developments have also occurred in the field of pharmacology.
Now, several new medicines work to perform their jobs better than their former counterparts. For this very reason, much advancement has been made in managing certain diseases and conditions in relation to former strategies.
The same could be applied to blood thinners. There are several types of blood thinners available in the markets now that are not only effective but overall safe to be used by older patients as well. (1)
Watch the Video for the Names of Blood Thinners
A brief overview of some of the popular blood thinners being used nowadays is given below:
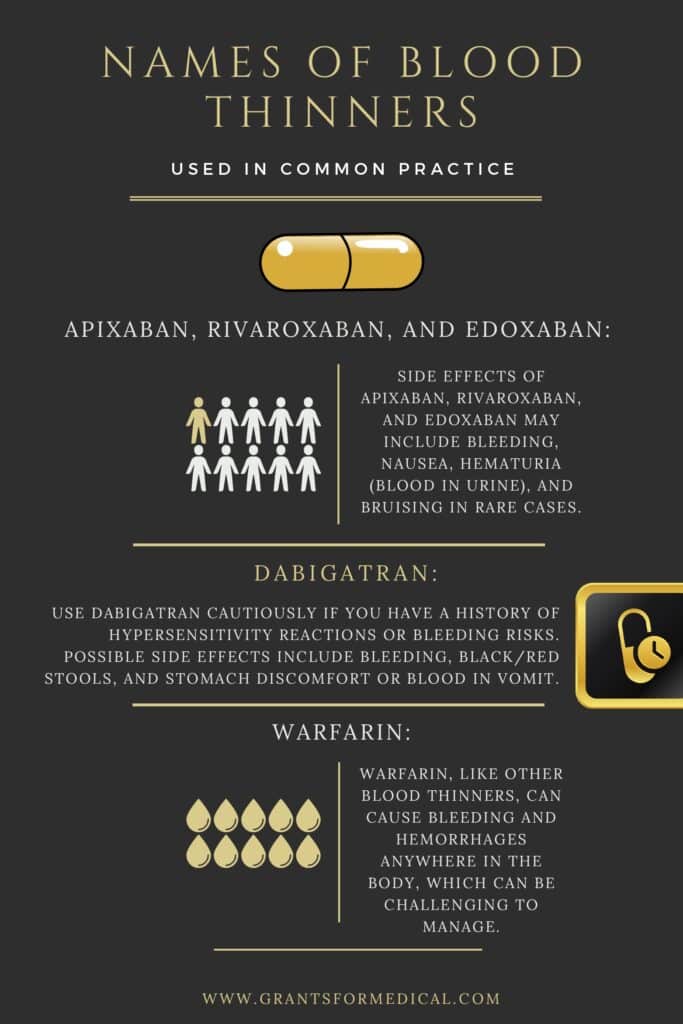
Apixaban, Rivaroxaban, and Edoxaban
The popularly used blood thinner Apixaban is available in markets called ‘Eliquis’. It is a type of blood thinner that is a selective inhibitor of the X-A clotting factor of the coagulation cascade. (2)
Factor X-A is responsible for converting prothrombin to thrombin, which ultimately leads to the formation of a blood clot. Therefore, when Apixaban is taken to inhibit this very step, there would be no clot formation where it is not needed. It is mostly used for patients with a diagnosis of atrial fibrillation or deep vein thrombosis. (3)
Rivaroxaban and Edoxaban are other blood thinners with the same mechanism of action as Apixaban. Rivaroxaban is indicated for the management of deep vein thrombosis, while edoxaban is used for reducing the risk of stroke in patients with atrial fibrillation.
- Side Effects:
Although Apixaban, Rivaroxaban, and Edoxaban are seen to be generally well-tolerated in individuals, it was also seen that there were some side effects of using these drugs.
Bleeding, nausea, hematuria (blood in urine), and bruise formation were some of the rare side effects noticed in some individuals.
See Also: Blood Thinners Side Effects
Dabigatran
Dabigatran is another popular blood thinner that is available in the market under the name Pradaxa. It is a potent inhibitor of thrombin. Because it is said to be a competitive inhibitor of thrombin, it was seen to bind to both clot-bound and free thrombin, impeding the formation of blood clots. (4)
However, Dabigatran is recommended to be used with extreme caution in patients with a history of hypersensitivity reactions and bleeding risks. (5)
- Side Effects:
The side effects associated with the usage of Dabigatran may include bleeding, black or red-colored stools, stomach discomfort, pain, or blood in the vomit.
Warfarin
Undoubtedly, one of the most popular and commonly used blood thinners is Warfarin. It is such a popularly used drug that it is widely employed for prophylactic purposes in patients with venous thromboembolism and other thromboembolic events. (6)
Warfarin is a Vitamin K antagonist. The liver uses vitamin K to synthesize most of the clotting factors involved in the coagulation cascade.
Therefore, when no active Vitamin K is present in the body, no clotting factors are available, and clot formation cannot occur accordingly.
Warfarin has been seen to significantly decrease the risk of death in patients already suffering from myocardial infarction, stroke, or thromboembolic events.
Warfarin is also available as an oral medicine. It is recommended to be taken once daily, and mostly later in the day, just so the physician can adjust its dose. (7)
- Side Effects:
Like every other blood thinner, Warfarin has some side effects. The most likely side effects associated with Warfarin are bleeding incidents and hemorrhage. Hemorrhages may occur anywhere in the body, and this is why it might be difficult to manage them when they occur.
Understanding the Coagulation Cascade
- The coagulation cascade is a normal cycle or mechanism performed by the body, where it works to form a clot as soon as an injury to the endothelium (the inner lining of blood vessels) occurs. It works to save you from any significant episode of bleeding and, thus, is helpful under such emergency circumstances. (8)
- However, doctors indicate blood thinners when a blood clot forms inside the bloodstream in a pathologic fashion caused by certain conditions.
- The coagulation cascade works under the influence of various factors, all of which are activated by their other counterparts. Once activated, each has a specific function that helps it reach its final stage of forming a clot.
- The coagulation pathway is divided into two parts – the extrinsic pathway and the intrinsic pathway.
- The intrinsic pathway depends on getting activated by blood coming into contact with a negatively charged surface, usually collagen, which is in the surround of blood vessels. It involves clotting factors XII, XI, IX, VIII, and V.
- The extrinsic pathway, on the other hand, gets activated when the tissue factor comes in contact (gets exposed) with the circulating blood. This pathway mainly involves the tissue factor and the clotting factor VII.
- The extrinsic and intrinsic pathways meet at one common point, where they both work to activate factor X. The clotting factor converts prothrombin (or factor II) to thrombin (factor IIA), which ultimately results in the conversion of fibrinogen to fibrin.
- The latter step produces a mesh containing platelets, giving architecture to the newly formed blood clot, impeding blood losses from the blood vessel.
Conclusions
To summarize it all, blood thinners are indeed a life-changing and beneficial option for people who are vulnerable to developing conditions such as venous thromboembolism, heart attack, and stroke.
Blood thinners are widely available in the market under many names, and their mechanisms of action differ. However, the primary purpose remains the same: to avoid the formation of blood clots in the bloodstream.
At the end of the day, if you have been declared as someone who is at risk of developing venous thromboembolism or heart attacks, then it is better if you visit a physician and follow the recommendations that best suit your condition to make sure that you live a healthy and happy life in the days to come!
Related Articles About Blood Thinners
See Also
What is Creatinine Level in Blood Tests?
Do Blood Thinners Decrease Blood Pressure?